A food allergy is a condition whereby someone’s immune system shows an overblown response to a normally harmless type of food. The most classic example includes difficulty in breathing and a sudden drop in blood pressure due to exposure to peanuts or seafood. In some severe cases, exposure to an allergen can result in a life-threatening reaction called anaphylaxis. The most common causes of anaphylaxis specific to food allergens include peanuts, tree nuts, fish, shellfish, and milk.
Although similar in nature, a food allergy is not the same as a food sensitivity or food intolerance. Individuals without clinical experience usually get confused when using these terms. Let’s clarify.
Food intolerance refers mostly to the incapability to process or digest certain foods and is not an immune system reaction. An example is someone experiencing caffeine intolerance. Food sensitivity, on the other hand, has no medical definition. Sometimes after eating certain foods, people feel uncomfortable and unwell. The symptoms are not life-threatening but can be quite troublesome, and include joint pain, stomach pain, fatigue, rashes, brain fog, etc. Gluten sensitivity or peanut sensitivity are good examples to describe food sensitivity. Careful observation and experimentation help physicians identify food sensitivities.
A food allergy is thus considered a “true” food allergy whose symptoms appear much faster than the symptoms associated with food intolerance/sensitivity. Physicians and dieticians always recommend their patients keep a food diary, taking note of the symptoms experienced after consuming the food and time of appearance. This information can assist a dietician or doctor in recognizing which foods are causing issues and what steps need to be taken moving forward.
It is seen that food allergies have been increasing in prevalence in the last two to three decades. The Food Allergy Research and Education (FARE) has found that food allergies affect about 32 million Americans including 5.6 million children under the age of 18. Though food allergies can affect anyone, they are found to be more common in children than in adults. According to one such study conducted in 2018, there are about 8% of children affected by food allergies in the United States. In other words, it affects 1 in 13 children or about 2 students per classroom.
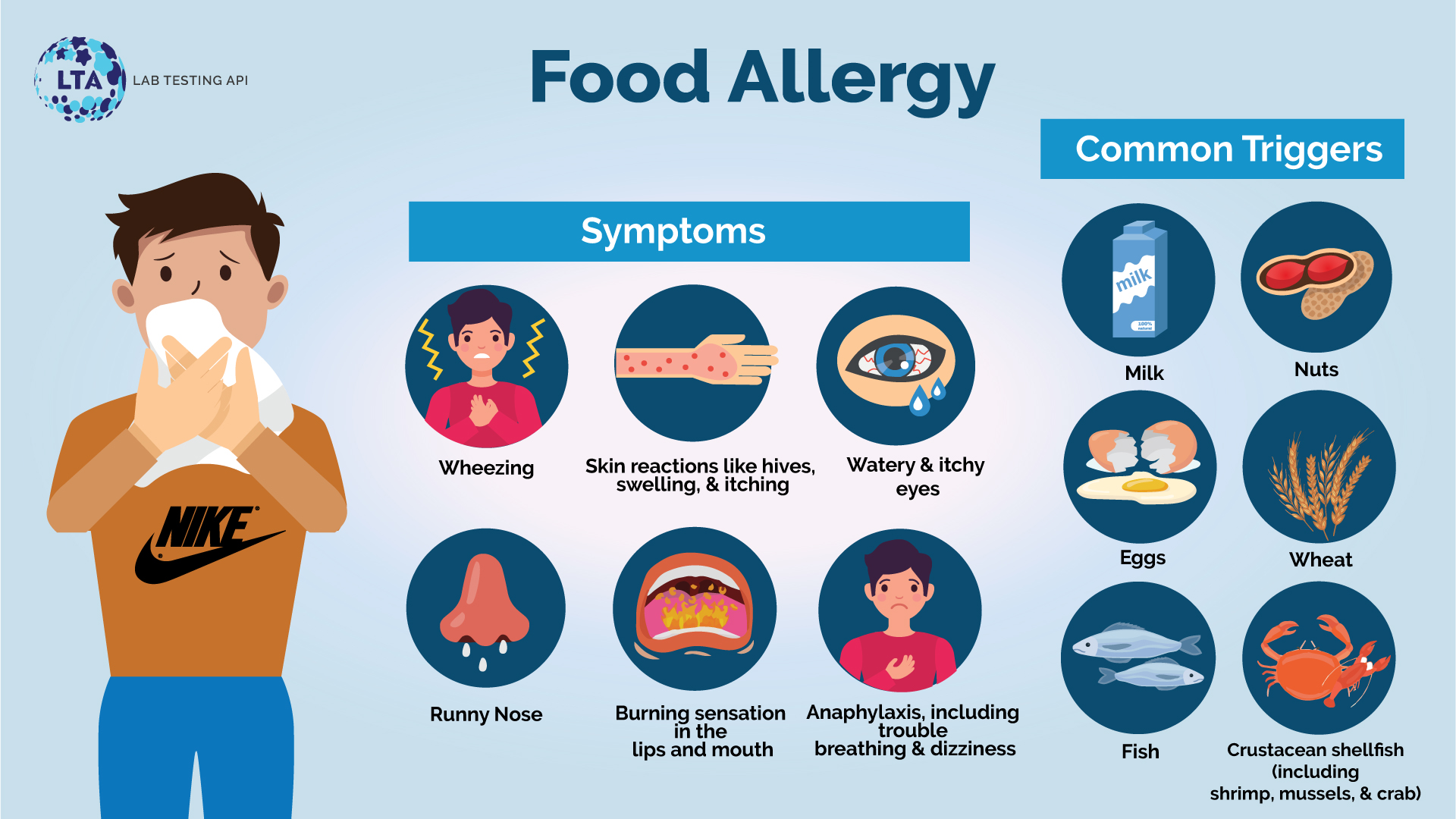
The onset of food allergy symptoms usually occurs immediately after consumption and could be mild to severe, and sometimes even life-threatening. The most common symptoms of food allergies are:
The associated risk of food allergies also increases if someone has:
The rise in food allergies in recent decades is an area of concern for food scientists and medical researchers across the globe. Though there could be many culprits, the most common allergenic foods that account for about 90% of all food allergies, (commonly referred to as the “big eight”) are (1,2):
Testing usually begins with your allergist or doctor performing a physical exam and asking about your symptoms. Careful observations and experimentations help physicians and dieticians identify which foods you are allergic to. An elimination diet is often prepared as a result. This is the process of removing certain foods that are believed to cause reactions from your diet for a few weeks. The foods are later reintroduced, one at a time, while the physician looks for symptoms that show a reaction. This is the gold standard for identifying food sensitivity but can also be utilized in identifying food allergies.
Oftentimes food allergies cannot be diagnosed merely by analyzing symptoms. Your healthcare practitioner may then request laboratory/medical tests for diagnosis and further treatment.
Doctors usually order a blood test and/or perform a skin prick food allergy test, both of which indicate whether food-specific immunoglobulin E (IgE) antibodies are present in your body. This would help doctors identify the presence of a food allergy. (3,4).
During a blood test, a healthcare professional will take a blood sample from a vein in your arm, using a small needle to check for substances called IgE antibodies in the blood. The human immune system makes different antibodies or immunoglobulins to protect the body from foreign invaders including bacteria, viruses, and allergens. Immunoglobulin E (IgE) is one of five classes of immunoglobulins/antibodies (A, G, M, D, and E). It is normally found in small amounts in the blood but its level increases when the body overreacts to allergens and its elevated levels can be inferred as the presence of an allergic disorder.
During a finger prick/finger stick method, the allergist places a drop of solution containing the food allergen, or the actual food itself (if a fruit or vegetable) on your forearm or back. By utilizing a small plastic probe or needle, the doctor would then gently prick or scratch the skin to allow a tiny amount of the solution/food to go beneath the skin’s surface. Positive results are usually indicated by a red, itchy bump at the injection site.
Lab Testing API offers a range of food allergy tests that an individual can order themselves online at discounted rates. All lab orders include a physician’s order. When you order your blood test through Lab Testing API, you may search for the required test or you may check the lab testing categories available on the website. Each test has its specific test instructions, including fasting instructions, for your convenience. This can be found under the “Testing Info” section of each test.
There is generally no cure for food allergies. Food allergies can be managed by avoiding or eliminating the foods causing the problem. It is always recommended to read the labels on packaged foods carefully. Additionally, notifying anyone who prepares or serves your food (waiters, babysitters, teachers, cafeteria workers, etc.) will reduce the risk of exposure to the food allergen.
The Centers for Disease Control and Prevention (CDC), in collaboration with the US Department of Education, several other federal agencies, and key stakeholders, have developed “Voluntary Guidelines for Managing Food Allergies In Schools and Early Care and Education Programs”. This Food Allergy Management Prevention Plan provides recommendations and practical information for preventing an allergic reaction and responding to a food allergy emergency.
The rise in food allergies in recent decades has been particularly noticeable around the globe. It would not be wrong to say that people are becoming more allergic to food. We do not yet have a cure or the ability to prevent food allergies from developing in the first place. However, one can manage and prevent the symptoms altogether by avoiding the food that’s causing the allergy. Once you and your healthcare provider have identified the foods to which you are sensitive, it is recommended to remove them from your diet. So as of now, managing food allergies is the best practice to follow.
Written by Dr. Shikha Sharma, Reviewed by Dr. Harshi Dhingra